Case Report: Radiography Induced Atrial Fibrillation
Leave a commentJune 4, 2013 by EmerJencyWEBB
A 69 yof presents to the ED with several days of crampy LLQ abdominal discomfort, diarrhea, and fever. Her vital signs are stable and her exam, although negative for peritonitis, reveals moderate tenderness in the left lower quadrant. Her kidney function is normal, so you decide to perform a CT abdomen/pelvis with contrast to r/o complications of diverticulitis (abscess, perforation), and other etiologies (most notably regional mesenteric ischemia).
A diagnosis of diverticulitis is made on CT imaging and there are no complicating features. Prior to discharge planning, a nurse alerts you that your patient’s heart rate has increased to the 130’s-160’s. An EKG is performed and looks like the tracing below:
The patient is otherwise stable and asymptomatic, so you take a little more history. She denies a history of structural or ischemic heart disease, arrhythmia, or pulmonary disease. On review of her chart, however, you find that she is currently being worked up by her PCP for a thyroid nodule. Aha! You now have it…
THE JOD-BASEDOW PHENOMENON AKA: Iodide-Induced Hyperthyroidism

It is named for Karl Adolph von Basedow, a German physician and the German word for iodine, “jod”.
Basically, this occurs because the iodinated contrast agent can put the production of thyroid hormone into overdrive, especially in susceptible populations with known or occult hyperthyroidism. Examples include Grave’s disease, hyperactive nodule, and multinodular goiter (1).
A typical dose of ICM contains approximately 13 500 μg of free iodide15 and 15 to 60 g of bound iodine1,15that may be liberated as free iodide in the body.15– 16 This represents an acute iodide load of 90 to several hundred thousand times the recommended daily intake of 150 μg.17 Sudden exposure to high iodide loads, given in other contexts, can disrupt thyroid hormone regulation, resulting in hypothyroidism (Wolff-Chaikoff effect)18– 19 or hyperthyroidism (jodbasedow).18,20
Arch Intern Med. 2012;172(2):153-159. doi:10.1001/archinternmed.2011.677.
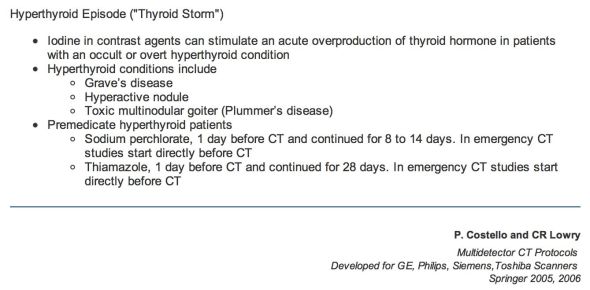
If you suspect or know your patient may be at risk for such an effect, there are pre- and post-imaging treatment options (1):
Atrial fibrillation is a complication that develops primarily in the elderly populations, and converts after the initiation of anti-thyroid therapy in 20-50% of patients (2). Rate control may be difficult in these patients without the use of such therapy. However, use of beta blockers (especially propanolol) instead of calcium channel blockers, can help inhibit the peripheral conversion of T4 to T3 and may provide the reduction you’re looking for.
Free Online Resources
1. http://www.mdct.net/eng/infoProtocols/cmSafety/otherReact/hyperthyroid.html
2. http://emedicine.medscape.com/article/767130-overview
3. http://jnm.snmjournals.org/content/38/11/1816.long
4. http://archinte.jamanetwork.com/article.aspx?articleid=1108674